Woman evicted from NHS hospital ward after being stuck for 18 months

BBC News
 BBC
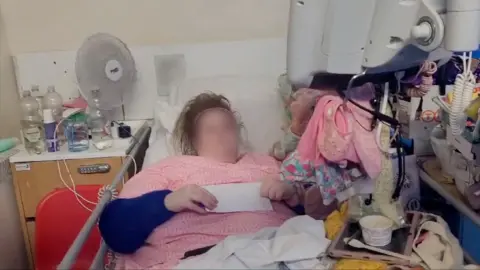
BBC“I feel very angry, upset, worthless, and like my mental health and my life does not matter,” says Jessie, propped up in a hospital bed.
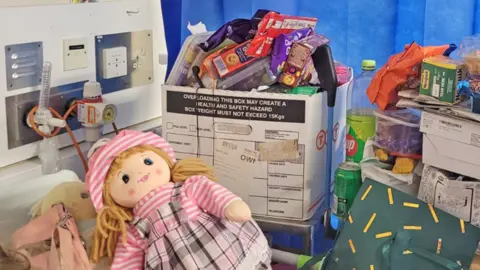
She is recording this in a video diary. Blue NHS curtains are drawn around the bed and all her possessions are stacked up in the tiny chaotic space this creates.
Among the piles of boxes and bags sit the dolls she holds to keep her calm.
Thirty-five-year-old Jessie spent 550 days in Northampton General Hospital. For nearly all that time, she was medically fit to leave but finding her a suitable place to go to was difficult.
The BBC has followed her story for more than five months as the NHS trust took costly High Court action against her, to have her evicted from the hospital bed she was occupying.
Jessie was eventually arrested and taken to a care home where she says she feels anxious.
Her story is an extreme example, but it demonstrates the acute pressures faced by a care system coping with more complex cases, the knock-on effect to the NHS, and how the person at the heart of it can feel lost.
North Northamptonshire Council, which is responsible for her housing and care, says it cannot comment because of an ongoing police investigation into Jessie’s behaviour.
The hospital says it “is not the best environment for patients who are not in need of acute medical care”.
The Department of Health and Social Care has told the BBC: “This is a troubling case which shows how our broken NHS discharge system is failing vulnerable people.”
Jessie was one of more than 70 people who contacted the BBC after reading about Matthew in Surrey – who would end up spending more than a year stuck on a hospital ward before being moved to a care home.
Most who wrote to us told of their struggles to find the social care they needed, some also faced long waits to get out of hospital.
At the start of January 2025, nearly 13,000 out of the more than 100,000 hospital beds in England were occupied by people who didn’t have a medical reason to be there, according to official figures.
For people delayed for more than a week, the most common reasons were a lack of social care available in their own homes, or a shortage of places in care or rehabilitation homes.
Such delays have become normal, say experts.
Jessie’s story
It is very rare for a patient to be taken to court by the NHS – Jessie’s is only the fourth case since 2006. So how did she come to be arrested in her hospital bed?
She arrived at Northampton General on 14 April 2023 needing treatment for cellulitis, a bacterial infection affecting the skin, which can be serious.
She uses a wheelchair and needs help with all her personal care. She has also been diagnosed with an emotionally unstable personality disorder.
Jessie likes games, arts and crafts, and trips to garden centres. She also finds life difficult and can be challenging to those trying to help her. When stressed, she self-harms and can threaten to harm others.
By the end of April, she was ready to be discharged from hospital, but was told she could not return to the nursing home where she had lived for nine years because it could no longer meet her needs.
Jessie – who is unable to work and reliant on benefits – became increasingly isolated stuck inside her hospital cubicle on the six-bedded ward. She says her mental health deteriorated further, people would stare at her and she felt safer with the curtains drawn.

From documents we have seen, and from what Jessie and her mother, Hilda, have told us, it was about a year before she was offered an alternative place by the local council.
Sarah Scobie, deputy director of research at the Nuffield Trust think tank, says patients stuck in hospital for three weeks or more, like Jessie, tend to need a lot of support, and the number of these cases is increasing.
With councils – who pay for most social care – financially squeezed and overstretched, many care homes and home-care providers are only given short-term funding, she says.
It is “difficult for them to establish services, recruit staff, train staff, invest in a service, if they don’t know whether that funding is going to continue,” she adds.
The government says it is providing an additional £26bn to help “shift the focus of care from hospital to community, and tackle delayed discharges by improving the links between the NHS and social care”.
It also says a review of adult social care led by Baroness Louise Casey, which starts work in April, will draw up a plan for a fair and affordable care system for the future.
In Jessie’s case, legal documents say the council investigated nearly 120 care places. Only one was offered to her.
This was a supported living flat in a nearby town, with two care staff initially present 24 hours a day.
But the town has upsetting memories for Jessie. She finds it too difficult to talk about, other than to say “bad things” happened.
She told us she was desperate to leave hospital, but the thought of going there made her feel suicidal. So, she refused the one place offered.

Under the 2014 Care Act, Jessie should be able to express a preference about where she lives.
She has mental capacity, but was assessed by the NHS as needing a professional advocate to support her in this, helping her understand the decisions she is asked to make and to explain her views to others.
Jessie was referred to an advocacy firm by the council, but in June 2024 her case was closed after she asked for a new advocate but then didn’t respond to further contact.
The health and care system is “convoluted, complicated, very bureaucratic” and it is easy for a patient’s voice to get lost, says Caroline Entwistle from the advocacy charity, VoiceAbility.
She believes an advocate can “take that pressure off the person who’s feeling quite overwhelmed” – but that funding for such services is not keeping up with demand.
The hospital did provide Jessie with mental health support while she was in her cubicle. But she believed no-one was listening to her.
“I explained all the reasons I wasn’t happy with [the accommodation],” she says, “but they just went ahead with it anyway.”
In August 2024, 16 months after she arrived, the hospital started legal action against Jessie to repossess the bed she was in.
She did not really understand what was happening, she says. Neither did her mother. They could not find a solicitor and had no advocate, so the first two hearings went ahead without anyone representing Jessie’s views.
The NHS trust argued a patient didn’t have the right to choose their placement, and that a hospital bed took up significant resource.
It said it had taken account of Jessie’s vulnerabilities throughout and the package of care offered by the council was significant, with staff present 24 hours a day to keep her safe.
A care plan, which detailed the support Jessie needed, was only given to the court at the final hearing. The date suggests the assessment was completed the day before. It also notes that “Jessie is unable to communicate effectively”.
At the final High Court hearing on 4 October, Jessie attended remotely from hospital. Within minutes she was overwhelmed and had to leave. Her mother struggled to speak for her.
The judge said Jessie could challenge the council’s assessment of whether the accommodation and care were right for her, but she could not remain in hospital “when she does not need a bed there, and has not needed one for over a year, and others do”.
He ruled that Jessie must leave hospital, and said “we must hope the transition goes smoothly”.
The hospital trust says it is committed to working with “care partners to provide the best possible care for those in our communities” in the place that “best suits their needs”.
The most recent data, from 2020-21, suggests a standard NHS hospital bed costs £345 per day. Adjusting for inflation, this would mean Jessie’s hospital stay is likely to have cost more than £200,000. We do not know how much the legal action cost.
Ten days after Jessie’s final hearing, 18 months after she arrived in hospital, the police arrested her. She spent several hours at a police station before being moved to the flat in the town that holds bad memories.
Police are investigating her for a number of alleged incidents, she told us, including for sending offensive emails shortly before she was evicted in October.
Since moving, Jessie says she has self-harmed and the police have been called on three occasions – once by Jessie, twice by staff.
“They don’t know what to do with me,” she says.
Jessie has recently been visited by a new advocate.
World News || Latest News || U.S. News
Source link




